Blood flow through the heart is a remarkable journey, a complex dance of chambers and valves that ensures the life-giving fluid reaches every corner of the body. This intricate process underpins our very existence, and understanding it unveils the secrets of our most vital organ.
From the heart's anatomy to the cardiac cycle's rhythmic beat, we will delve into the intricacies of blood flow, unraveling the mechanisms that drive this vital process.
Anatomy of the Heart
The heart is a muscular organ located in the chest, responsible for pumping blood throughout the body. It consists of four chambers: two atria (singular: atrium) and two ventricles. The atria are the upper chambers, while the ventricles are the lower chambers.
The heart valves play a crucial role in ensuring the proper flow of blood through the heart. There are four main heart valves: the tricuspid valve, the pulmonary valve, the mitral valve, and the aortic valve. These valves open and close in a coordinated manner to prevent backflow of blood.
Role of the Heart in Blood Circulation
The heart plays a central role in the circulatory system, which is responsible for transporting blood, oxygen, and nutrients throughout the body. The heart pumps blood from the atria to the ventricles, and then out to the body through the arteries.
The blood then returns to the heart through the veins, completing the circulatory cycle.
Cardiac Cycle
The cardiac cycle refers to the sequence of events that occur during one complete heartbeat. It consists of two main phases: systole and diastole.
The cardiac cycle is controlled by electrical impulses generated by the heart's sinoatrial node (SA node). These impulses spread through the heart, causing the atria to contract (atrial systole) and then the ventricles to contract (ventricular systole). The relaxation of the atria and ventricles is known as atrial diastole and ventricular diastole, respectively.
Relationship between Electrical and Mechanical Events
The electrical events of the cardiac cycle are closely linked to the mechanical events. The electrical impulses generated by the SA node trigger the release of calcium ions from the sarcoplasmic reticulum, which causes the heart muscle cells to contract.
The contraction of the heart muscle cells then leads to the mechanical events of the cardiac cycle, such as the ejection of blood from the heart.
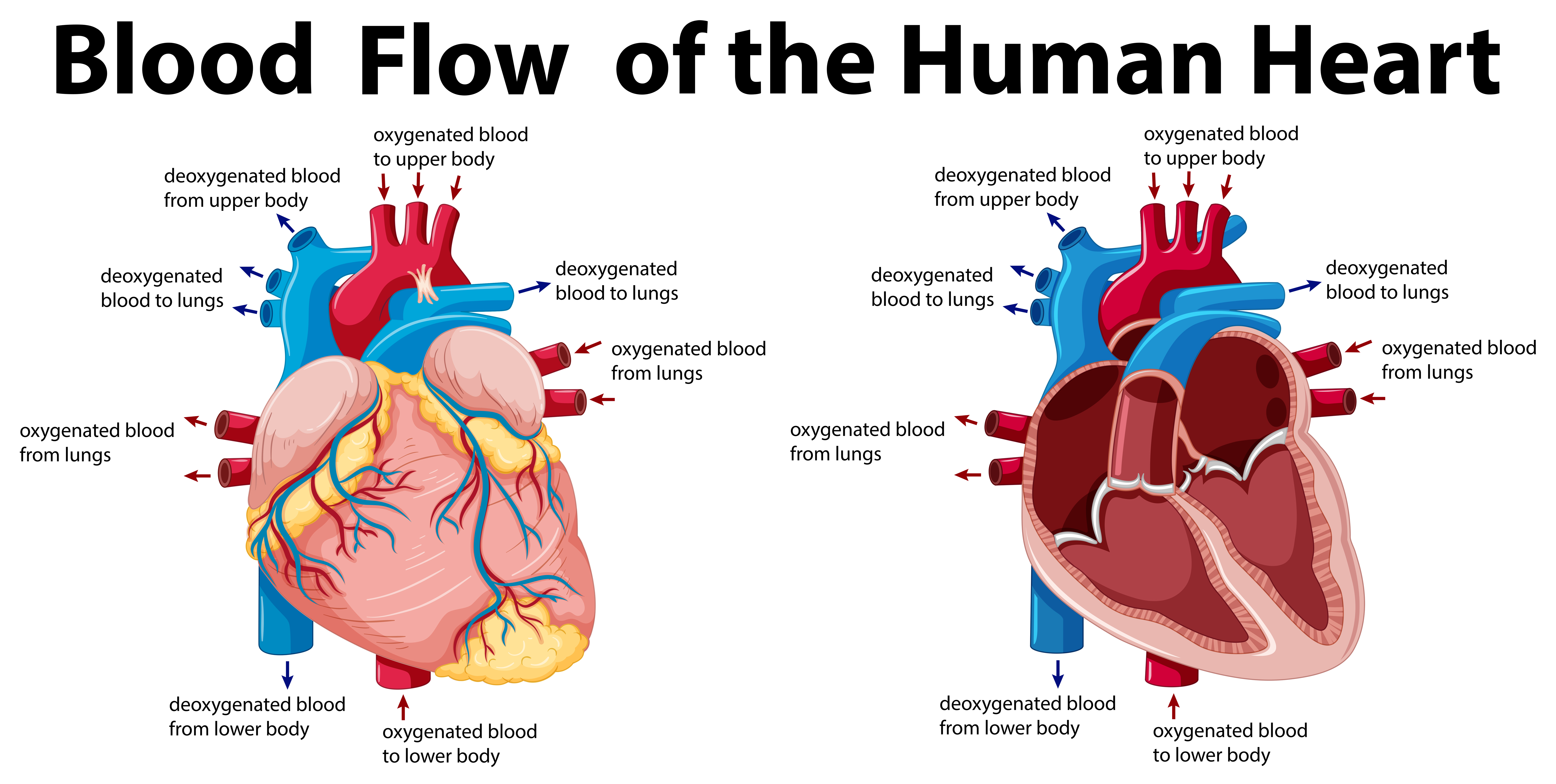
Blood Flow through the Heart
The heart pumps blood throughout the body, delivering oxygen and nutrients to the cells and removing waste products. The path of blood flow through the heart is as follows:
- Deoxygenated blood from the body enters the heart through the superior and inferior vena cavae.
- The blood enters the right atrium, which contracts and pumps the blood into the right ventricle.
- The right ventricle contracts and pumps the blood into the pulmonary artery, which carries the blood to the lungs.
- In the lungs, the blood picks up oxygen and releases carbon dioxide.
- The oxygenated blood returns to the heart through the pulmonary veins.
- The blood enters the left atrium, which contracts and pumps the blood into the left ventricle.
- The left ventricle contracts and pumps the blood into the aorta, which carries the blood to the body.
Blood pressure is generated by the contraction of the heart. When the heart contracts, it increases the pressure in the arteries, which pushes the blood through the body. The pressure in the arteries is highest when the heart contracts (systolic pressure) and lowest when the heart relaxes (diastolic pressure).
Coronary Circulation
The coronary circulation is a system of blood vessels that supplies oxygenated blood to the heart muscle. It is composed of the coronary arteries, which branch off from the aorta, and the coronary veins, which drain into the right atrium.The coronary arteries are divided into two main branches: the left coronary artery and the right coronary artery.
The left coronary artery supplies blood to the left ventricle, left atrium, and interventricular septum. The right coronary artery supplies blood to the right ventricle, right atrium, and sinoatrial node.The coronary veins are divided into two main branches: the great cardiac vein and the middle cardiac vein.
The great cardiac vein drains blood from the left ventricle, left atrium, and interventricular septum. The middle cardiac vein drains blood from the right ventricle and right atrium.Coronary blood flow is essential for the proper functioning of the heart. If the coronary arteries become blocked, it can lead to a heart attack.
A heart attack occurs when the heart muscle is deprived of oxygen and nutrients, which can damage or kill the heart muscle.
Regulation of Heart Rate
The heart rate is regulated by a complex interplay of neural, hormonal, and intrinsic factors. The autonomic nervous system, consisting of the sympathetic and parasympathetic branches, plays a central role in regulating heart rate.
As blood flows through the heart, it carries oxygen and nutrients to the body's cells. However, the presence of alcohol in the blood can disrupt this process. Blood alcohol level (BAL) is a measure of the amount of alcohol in a person's bloodstream.
High BAL can lead to impaired judgment, slowed reaction times, and difficulty concentrating. This can have a negative impact on the heart's ability to pump blood effectively, potentially leading to cardiovascular problems.
Sympathetic Nervous System
The sympathetic nervous system increases heart rate by releasing norepinephrine, which binds to beta-1 adrenergic receptors on cardiac myocytes. This binding stimulates the production of cyclic adenosine monophosphate (cAMP), leading to increased calcium influx and enhanced contractility. The sympathetic nervous system is activated in response to stress, exercise, and other situations that require increased cardiac output.
Parasympathetic Nervous System
The parasympathetic nervous system decreases heart rate by releasing acetylcholine, which binds to muscarinic receptors on cardiac myocytes. This binding activates potassium channels, leading to membrane hyperpolarization and decreased calcium influx. The parasympathetic nervous system is activated during rest and relaxation, and it helps to conserve energy and prevent excessive heart rates.
Hormones
Several hormones also affect heart rate. Epinephrine and norepinephrine, released by the adrenal glands, stimulate the sympathetic nervous system and increase heart rate. Thyroid hormones increase the metabolic rate and can lead to increased heart rate. Conversely, vagal tone, mediated by the parasympathetic nervous system, decreases heart rate.
Other Factors
Other factors that can affect heart rate include body temperature, blood pressure, and electrolyte balance. Increased body temperature and decreased blood pressure can lead to increased heart rate, while electrolyte imbalances, such as hyperkalemia and hypokalemia, can cause abnormal heart rhythms and affect heart rate.
Cardiac Output
Cardiac output (CO) is the volume of blood pumped by each ventricle per minute. It is calculated by multiplying heart rate (HR) by stroke volume (SV).
CO = HR × SV
Cardiac output is a measure of the heart's pumping efficiency and is essential for maintaining adequate blood flow to the body's tissues.
Factors Affecting Cardiac Output
- Heart rate:Increased heart rate increases cardiac output, while decreased heart rate decreases cardiac output.
- Stroke volume:Increased stroke volume increases cardiac output, while decreased stroke volume decreases cardiac output.
- Preload:Increased preload (the amount of blood in the ventricles at the end of diastole) increases stroke volume and cardiac output, while decreased preload decreases stroke volume and cardiac output.
- Afterload:Increased afterload (the resistance against which the ventricles must pump) decreases stroke volume and cardiac output, while decreased afterload increases stroke volume and cardiac output.
- Contractility:Increased contractility (the force of ventricular contraction) increases stroke volume and cardiac output, while decreased contractility decreases stroke volume and cardiac output.
Heart Failure
Heart failure is a condition in which the heart is unable to pump enough blood to meet the body's needs. This can be caused by a variety of factors, including:
- Coronary artery disease
- High blood pressure
- Diabetes
- Obesity
- Smoking
- Alcohol abuse
- Family history of heart failure
Symptoms of heart failure can include:
- Shortness of breath
- Fatigue
- Swelling in the feet, ankles, and legs
- Chest pain
- Lightheadedness or dizziness
- Confusion
- Nausea or vomiting
There are two main types of heart failure:
- Systolic heart failure occurs when the heart is unable to pump enough blood out of the ventricles.
- Diastolic heart failure occurs when the heart is unable to fill with enough blood during diastole.
Heart failure is a serious condition that can lead to death. Treatment for heart failure includes medications, lifestyle changes, and sometimes surgery.
Imaging Techniques for Assessing Blood Flow through the Heart
Imaging techniques play a crucial role in assessing blood flow through the heart, providing detailed information about cardiac structure and function. These techniques include echocardiography, cardiac MRI, and other specialized modalities. Each technique offers unique advantages and disadvantages, making them suitable for different clinical scenarios.
Echocardiography, Blood flow through the heart
Echocardiography is a non-invasive imaging technique that uses ultrasound waves to create images of the heart. It is widely used to assess cardiac structure, function, and blood flow patterns. Advantages of echocardiography include its portability, real-time imaging capabilities, and relatively low cost.
However, it can be limited by image quality, especially in obese patients or those with poor acoustic windows.
Cardiac MRI
Cardiac MRI (CMR) utilizes magnetic resonance imaging to produce high-resolution images of the heart. CMR provides excellent visualization of cardiac anatomy, including the chambers, valves, and surrounding structures. It also allows for the assessment of blood flow patterns and myocardial perfusion.
Advantages of CMR include its non-invasive nature, lack of ionizing radiation, and ability to quantify cardiac function accurately. However, it is more expensive and time-consuming than echocardiography and requires specialized equipment and expertise.
Other Imaging Techniques
Other imaging techniques used for assessing blood flow through the heart include:
- Nuclear medicine scans: These scans use radioactive tracers to visualize blood flow and myocardial perfusion.
- Computed tomography (CT) angiography: This technique combines CT imaging with contrast agents to visualize coronary arteries and assess blood flow.
- Positron emission tomography (PET): PET scans use radioactive tracers to assess myocardial metabolism and blood flow.
Interventions to Improve Blood Flow through the Heart
Interventions to improve blood flow through the heart aim to address underlying causes of reduced blood flow, such as coronary artery disease, heart valve disorders, or cardiomyopathy. These interventions range from lifestyle modifications to surgical procedures, and the choice of intervention depends on the severity and cause of the blood flow restriction.
The primary goal of these interventions is to restore adequate blood supply to the heart muscle, ensuring its proper function and preventing further damage. Understanding the risks and benefits of each intervention is crucial for informed decision-making and optimal patient outcomes.
Lifestyle Modifications
Lifestyle modifications, such as adopting a heart-healthy diet, regular exercise, smoking cessation, and stress management, can significantly improve blood flow through the heart. These measures aim to reduce risk factors for heart disease, including high blood pressure, high cholesterol, and obesity, which can contribute to the development of coronary artery disease.
Regular exercise helps strengthen the heart muscle, improve blood vessel function, and lower blood pressure. Quitting smoking is essential as nicotine constricts blood vessels and increases the risk of blood clots. Managing stress through techniques like yoga, meditation, or deep breathing can help lower blood pressure and improve overall cardiovascular health.
Medications
Medications play a crucial role in improving blood flow through the heart. Several classes of drugs are commonly used, including:
- Antiplatelet agents, such as aspirin or clopidogrel, prevent blood clots from forming in the arteries.
- Statins, such as atorvastatin or simvastatin, lower cholesterol levels and reduce the buildup of plaque in the arteries.
- Beta-blockers, such as metoprolol or carvedilol, slow the heart rate and lower blood pressure, reducing the workload on the heart.
- ACE inhibitors, such as lisinopril or ramipril, dilate blood vessels and lower blood pressure.
- Nitrates, such as nitroglycerin, relax blood vessels and improve blood flow to the heart.
Surgical Interventions
Surgical interventions may be necessary when lifestyle modifications and medications are insufficient to improve blood flow through the heart. Common surgical procedures include:
- Coronary artery bypass grafting (CABG): A procedure where a healthy blood vessel from another part of the body is grafted onto the blocked coronary artery, creating a new pathway for blood flow.
- Percutaneous coronary intervention (PCI): A minimally invasive procedure where a stent is inserted into the blocked coronary artery to widen it and improve blood flow.
- Heart valve replacement or repair: A procedure to replace or repair damaged or diseased heart valves, ensuring proper blood flow through the heart chambers.
Risks and Benefits
Each intervention has its own risks and benefits that should be carefully considered. Lifestyle modifications generally have minimal risks and can significantly improve blood flow through the heart. Medications may have side effects, such as dizziness, nausea, or muscle pain, but they can effectively reduce the risk of heart events and improve blood flow.
As blood flows through the heart, it is pumped through a series of chambers, including the atria and ventricles. The flow of blood is regulated by valves, which prevent backflow. The true blood cast is a group of actors who have played characters in the popular television series True Blood.
The series follows the lives of vampires and humans in the fictional town of Bon Temps, Louisiana. The blood flow through the heart is essential for the body to function properly, as it delivers oxygen and nutrients to the tissues and organs.
Surgical interventions carry higher risks, including bleeding, infection, and complications during or after surgery. However, these procedures can be life-saving in cases of severe blood flow restriction or heart failure. The decision to undergo surgery is made in consultation with a healthcare professional after carefully weighing the risks and benefits.
Clinical Applications
Understanding blood flow through the heart is essential for diagnosing and treating heart disease. By comprehending the normal patterns of blood flow, physicians can identify abnormalities that may indicate underlying cardiac issues.
Cardiac imaging techniques, such as echocardiography and magnetic resonance imaging (MRI), allow visualization of blood flow patterns within the heart. These images can reveal areas of reduced or obstructed flow, helping diagnose conditions like valvular heart disease, coronary artery disease, and congenital heart defects.
Diagnosis of Heart Disease
- Echocardiography:Uses ultrasound to create images of the heart, showing blood flow patterns and identifying abnormalities like valve dysfunction or chamber enlargement.
- MRI:Provides detailed cross-sectional images of the heart, allowing assessment of blood flow in the chambers, valves, and coronary arteries.
- Cardiac Catheterization:A minimally invasive procedure that involves inserting a catheter into the heart to measure pressure gradients and visualize blood flow.
Treatment of Heart Disease
Understanding blood flow through the heart guides treatment decisions for heart disease. For example, in coronary artery disease, where blood flow to the heart muscle is obstructed, interventions such as angioplasty or bypass surgery aim to restore normal blood flow.
The heart's rhythmic contractions pump blood throughout the body, delivering oxygen and nutrients to cells. When blood pressure drops below normal levels, symptoms like dizziness, fainting, and fatigue may arise. Low blood pressure symptoms can result from various factors, including dehydration, blood loss, or certain medications.
Understanding these symptoms and their underlying causes is crucial for maintaining cardiovascular health and ensuring adequate blood flow through the heart.
In valvular heart disease, where valves malfunction, surgical or transcatheter procedures may be performed to repair or replace the affected valves, improving blood flow through the heart.
Future Directions in Research
Research on blood flow through the heart has made significant progress in recent years, but there are still many areas where further research is needed. One area of focus is the development of new imaging techniques to visualize blood flow in the heart.
These techniques could help to identify and diagnose heart problems at an early stage.Another area of research is the development of new treatments for heart problems. These treatments could include new drugs, devices, or surgical techniques. The goal of these treatments is to improve blood flow to the heart and prevent heart problems from developing.
Research on the Microcirculation
The microcirculation is the network of small blood vessels that supply blood to the tissues and organs of the body. The microcirculation is responsible for delivering oxygen and nutrients to the cells and removing waste products.Research on the microcirculation is important because it can help us to understand how blood flow is regulated in the body.
This knowledge could lead to new treatments for heart problems and other diseases that affect the microcirculation.
Research on the Role of Blood Flow in Heart Disease
Heart disease is the leading cause of death in the United States. Blood flow plays a key role in the development of heart disease. For example, high blood pressure can damage the blood vessels that supply blood to the heart.
This can lead to a heart attack.Research on the role of blood flow in heart disease is important because it can help us to develop new strategies to prevent and treat heart disease.
Last Recap
Blood flow through the heart is a testament to the body's exquisite design, a symphony of biological precision. Understanding this intricate process empowers us to appreciate the marvels of our own physiology and equips us with the knowledge to safeguard our heart's health.
FAQ Insights: Blood Flow Through The Heart
What is the cardiac cycle?
The cardiac cycle refers to the sequential events that occur during one complete heartbeat, including atrial and ventricular contraction and relaxation.
How is blood pressure generated?
Blood pressure is generated by the force of the heart's contractions against the resistance of the blood vessels.
What is coronary circulation?
Coronary circulation refers to the network of blood vessels that supply oxygen-rich blood to the heart muscle itself.
Tags: #Blood Flow #Blood pressure #Cardiac Cycle #Coronary Circulation #Heart





